What Is Osteoarthritis?
The key feature of OA is the gradual breakdown of the articular cartilage that lines the ends of bones in a joint. Cartilage serves as a smooth, cushioning surface that allows the joint to move without friction. In OA, this cartilage becomes damaged and progressively thins, leading to joint pain, stiffness, and reduced function.
As the cartilage deteriorates, the underlying bone may undergo changes, such as the formation of bone spurs or osteophytes. This increased density in response to the stress placed on the joint. These bony changes can further contribute to joint pain and discomfort.
What Are The Symptoms?

Joint Pain
The hallmark of osteoarthritis is pain in the affected joint. This pain is often described as a deep ache and may worsen with activity.
Stiffness
Affected joints can become stiff, making it challenging to move them, especially in the morning or after periods of inactivity.

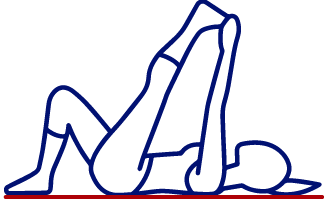
Limited Range of Motion
As osteoarthritis progresses, joint movement may be restricted.
Swelling
Inflammation of the affected joint can lead to swelling.

Grating Sensation
Some people experience a grating or crunching sensation when using the affected joint.
Causes and Risk Factors
Knowing the causes and risk factors for osteoarthritis is essential for effective prevention and management of this degenerative joint condition, providing valuable insights into strategies to maintain joint health and overall well-being.
What Are The Causes?
Osteoarthritis occurs when the protective cartilage that cushions the ends of your bones deteriorates over time. Several factors contribute to the development of osteoarthritis:
- Prior surgery: The risk of developing osteoarthritis increases with certain procedures like ACL repair, spinal fusions, and other surgical interventions.
- Genetics: Family history can play a role in OA development.
- Joint Injuries: Previous joint injuries or overuse can contribute to osteoarthritis in those joints.
- Sports and Physical Activity: Participation in high-impact sports or activities that place excessive stress on the joints, such as running or contact sports, can increase the risk of joint injury and OA.
- Metabolic syndrome: High blood pressure, blood sugar, excess waist fat, and abnormal cholesterol heighten OA risk in weight-bearing joints like knees and hips.
- Obesity: Excess weight can put additional stress on weight-bearing joints, such as the knees and hips.
- Diabetes: Diabetes, particularly type 2 diabetes, is associated with an increased risk of OA. High blood sugar levels can lead to inflammation and damage to joint tissues, contributing to OA development.
- Gout: A condition marked by uric acid crystal buildup in joints, causing inflammation and pain, can affect joint health and increase the risk of developing OA in the affected joints.
What Are The Risk Factors?
- Age:
- Gender: Osteoarthritis is more common in women, particularly after menopause.
- Inactivity: A sedentary lifestyle can lead to muscle weakness and joint stiffness, increasing the risk of OA.
- Occupational Hazards: Certain occupations that involve repetitive joint movements, heavy lifting, or kneeling may increase the risk of OA. People in physically demanding jobs may be more susceptible to OA.
- Posture: Poor posture can increase the risk factors for developing osteoarthritis (OA) by placing additional stress on your joints and affecting the overall biomechanics of your body.
How Is Osteoarthritis Diagnosed?
To diagnose osteoarthritis, healthcare providers typically consider a combination of factors:
- Physical Examination: A healthcare professional will examine the affected joint, looking for signs of OA, such as tenderness, swelling, and restricted movement.
- Medical History: Your doctor will inquire about your symptoms and medical history.
- Imaging: X-rays and MRI scans can reveal joint damage and help confirm an osteoarthritis diagnosis.
- Blood Tests: In some cases, blood tests may be conducted to rule out other conditions.

How Can We Treat Osteoarthritis
Osteoarthritis is a chronic condition, but there are various treatment options available to manage its symptoms and improve your quality of life. Some of these treatments include:
Schedule Your Appointment Today
Contact us today to book a free 15-minute consultation with our Chiropractor in Highlands Ranch! We look forward to getting you on the path to optimal health and wellness.